“Only a single 25 bp deletion in one candidate gene triggered the sudden cardiac arrest crisis in India. Studies suggest that millions of people are at risk.”
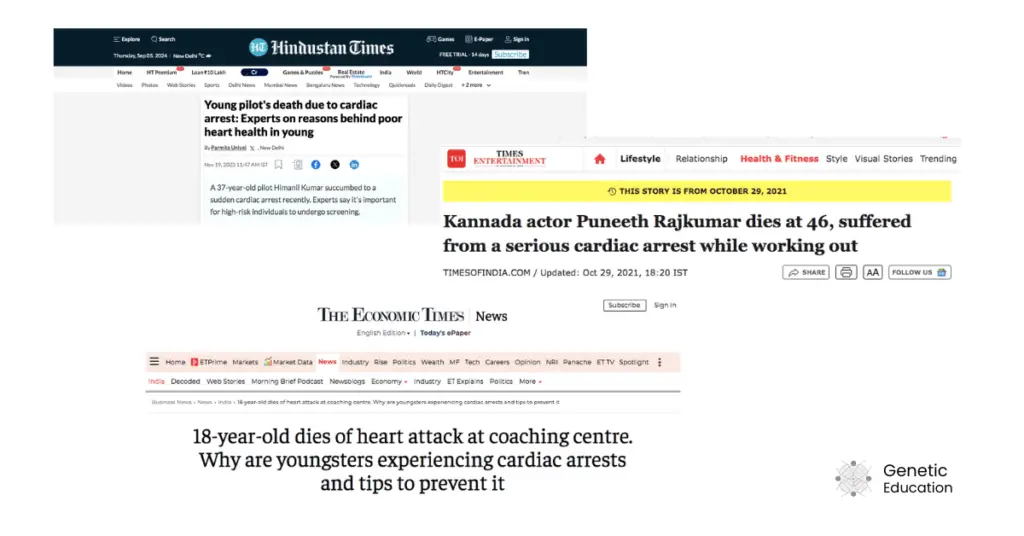
Known personalities like Punith Rajkumar, Singer KK, Raju Shrivastav, and Sidharth Shukla died at a young age due to sudden cardiac arrest. Indian Air Force pilot Himani (Age 37), a young boy in the coaching institute and many in the gym (below 40 years) died due to cardiac arrest.
In addition, thousands of unreported cases witnessed cardiac arrest as a crisis in the young Indian population. The COVID pandemic has been blamed initially as a main source of heart weakening, however, the reason was rooted 30,000 years before!
A gene known as MYBPC3 evolved 30,000 years ago affecting millions of lives in India and whole South Asia with a single mutation.
Catch the story of sudden cardiac arrest (SCA) and the role of genetic factors in this crisis.
Stay tuned.
Related articles:
- Lord Birsa Returns: Meet A CRISPR-Based Gene Therapy BIRSA 101
- An Expert Explains Why the 385-Million-Year Symbiosis Between Corals and Algae Is At Risk
- Newsletter 11: Top 5 Genetic Research and Stories of This Week 4
- Newsletter 09: Top 5 Genetic Research and Stories of This Week 2
- Your Eyes Age Faster Than You- Here is Why
Disclaimer: The content presented herein has been compiled from reputable, peer-reviewed sources and is presented in an easy to understand manner for better comprehension. A complete list of sources is provided after the article for reference.
Key Topics:
What is Sudden Cardiac Arrest?
In simple words, it’s a condition in which the heart unexpectedly stops beating. Eventually, it stops immediate blood flow to the brain and other body parts. It is a medical emergency that occurs without any signs.
Patients may feel breathing problems, collapse suddenly and lose consciousness. Pulse and breathing movement become zero immediately. The patient should be treated immediately.
Most of the SCA leads to death. In recent times, its high prevalence has been reported in young people in India. Studies showed that due to the imbalance in the heart’s activity led by inefficient myosin and actin activity, the present scenario arises.
Some associated statistics
- The global leading cause of death is cardiovascular disease.
- The annual incidence of sudden cardiac arrest is 53 per 1,00,000 in India.
- Sudden cardiac arrest is 4.6 times higher in men compared to women.
How does it happen?
The MYBPC3 gene codes myosin-binding protein 3. It’s a type of cardiac protein that regulates the cardiac or heart muscle contraction. The process of present rhythmic heart movement is achieved through the interaction of the MYBPC3 protein with myosin and actin filaments.
By ensuring the perfect structure and function of myosin and actin, MYBPC3 also ensures heart contraction and relaxation efficiently. Mutation in MYBPC3 produces an inefficient myosin-binding protein.
The mutant protein can not govern the overall contraction and relaxation in the heart and leads to muscle weakening. The condition becomes worse after the 30s and individuals face sudden cardiac arrest during hyper-cardiac activities like exercise, mental stress or even live concerts.
What is the MYBPC3 gene?
A gene is a coding part of the genome that synthesizes a protein. Among the 3.2 billion nucleotides of the human genome, 2 to 3% have been designated as genes. 20,000 to 25,000 genes are annotated to date.
Structurally genes are made up of exons and introns which are coding and non-coding sequences, respectively. Introns are removed from the final transcript product, only the exons express and produce a protein.
MYBPC3 encodes Myosin Binding Protein 3. It is located on chromosome 11 at 11p11.2. It has 35 exons and a total gene length of 21Kb. The official NCBI gene report suggests that it is exclusively expressed in the heart muscle.
The present myosin-associated protein regulates cardiac contraction. So mutations in the MYBPC3 gene are directly associated with various types of cardiomyopathies. Sakthivel (2001) reported cardiomyopathy-associated 25 bp deletion in this gene.
The deletion is reported in the intron 32 and between the exon 32 and 33. Though various other MYBPC3 gene mutations are associated with various types of cardiomyopathy, the 25 bp deletion has been reported with higher frequency.
The present mutation follows autosomal dominant inheritance. That means a single mutant gene copy is sufficient enough to show the symptoms. Noteworthy, homozygous dominant with two mutant alleles can not live longer than 5 years.
Thangaraj K et al. showed that this lethal gene mutation is commonly found in Southeast Asia (India, Pakistan, Sri Lanka and others) but not in other parts of the world.
Adding to this, their report published in Nature also suggests that the present gene mutation is associated with 44% of sudden cardiac arrest after the age of reproduction.
Candidate gene in Southeast Asia
Things become interesting after Sakthivel et al. (2001) study. Two unrelated cases have been diagnosed with the same 25 bp deletion in the MYBPC3 gene, and guess what! Those two cases belonged to South Asia!
Kumarasamy Thangaraj and co-workers at CCMB deciphered that individuals with a 25 bp MYBPC3 gene mutation have a 7-fold higher risk for cardiomyopathy, particularly in Southeast Asia.
Furthermore, carriers sense disease symptoms in their 30s. Two meta-studies, one case-control and another on various populations across India, revealed that the present mutation occurs at a significantly higher frequency in patients suffering from heart problems compared to controls.
Another study on 6273 unrelated patients demonstrated that the frequency of the present candidate mutation is 4%. This means that out of 6273 patients ~251 cases have MYBPC3 gene 25 bp deletion. That is indeed quite high!
Scattered studies across the world in 26 different countries further witnessed that the present genetic mutation is common in India, Pakistan, Sri Lanka and other countries of the Indian subcontinent.
This certainly shows it was spread from India to other South Asian countries in the past.
Epigenetic landscape:
A homozygous dominant is a very short-lived condition, as aforesaid. However, for carriers, it is crucial to know how it can happen and how it can be prevented.
Carriers carry one mutant and one normal copy of the MYBPC3 gene. If, somehow, a person manages to produce higher copies of the normal MYBPC3 allele, then the condition can be managed.
Epigenetic research evidence that gene copy numbers also matter! A person’s adverse lifestyle such as eating junk food, bad cholesterol intact, lack of physical activities and mental stress increases the level of mutant MYPBC3 gene copy.
Henceforth, lifestyle factors are as important as genetic ones! Maintaining a healthy lifestyle can result in a higher copy number of a normal gene. Means, you are risk-free!
So even if a person is diagnosed as a MYBPC3 gene carrier, no need to worry! Healthify your epigenetic profile. That’s it! However, the genetic predisposition associated with the MYBPC3 gene is lifelong, so long-term care is necessary.
Related article: Epigenetics 101: What is Epigenetics and How Does It Work?
Wrapping up:
The 30 bp MYBPC3 gene mutation is gradually spreading in the Indian subcontinent. And its effects are already being noticed. It is important to note, however, that other mutations are also linked with the SCA.
However, it is noteworthy to know that other mutations are also associated with the SCA.
Studies demonstrate that healthy lifestyles can regulate the MYBPC3 epigenetic profile, offering a chance of improved survival. Nonetheless, genetic counseling and testing are essential to prevent further spread of the mutation.
Sources:
Kuster DW, Sadayappan S. MYBPC3’s alternate ending: consequences and therapeutic implications of a highly prevalent 25 bp deletion mutation. Pflugers Arch. 2014 Feb;466(2):207-13. doi: 10.1007/s00424-013-1417-7. Epub 2013 Dec 11. PMID: 24327208; PMCID: PMC3946836.
Sadayappan S, Puckelwartz MJ, McNally EM. South Asian-Specific MYBPC3Δ25bp Intronic Deletion and Its Role in Cardiomyopathies and Heart Failure. Circ genom Precis Med. 2020 Jun;13(3):e002986. doi: 10.1161/CIRCGEN.120.002986.
Bazrafshan S, Sibilia R, Girgla S, Viswanathan SK, Puckelwartz MJ, Sangha KS, Singh RR, Kakroo M, Jandarov R, Harris DM, Rubinstein J, Becker RC, McNally EM, Sadayappan S. South Asian-Specific MYBPC3Δ25bp Deletion Carriers Display Hypercontraction and Impaired Diastolic Function Under Exercise Stress. Front Cardiovasc Med. 2021 Dec 23;8:766339. doi: 10.3389/fcvm.2021.766339. PMID: 35004883; PMCID: PMC8733148.
Deo R, Albert CM. Epidemiology and genetics of sudden cardiac death. Circulation. 2012 Jan 31;125(4):620-37. doi: 10.1161/CIRCULATIONAHA.111.023838.
Bazrafshan S, Sibilia R, Girgla S, Viswanathan SK, Puckelwartz MJ, Sangha KS, Singh RR, Kakroo M, Jandarov R, Harris DM, Rubinstein J, Becker RC, McNally EM, Sadayappan S. South Asian-Specific MYBPC3Δ25bp Deletion Carriers Display Hypercontraction and Impaired Diastolic Function Under Exercise Stress. Front Cardiovasc Med. 2021 Dec 23;8:766339. doi: 10.3389/fcvm.2021.766339.
Harper, Andrew R, et al. “Reevaluation of the South Asian MYBPC3 Δ25bp Intronic Deletion in Hypertrophic Cardiomyopathy.” Circulation Genomic and Precision Medicine, vol. 13, no. 3, 1 June 2020, https://doi.org/10.1161/circgen.119.002783. Accessed 5 Sept. 2024.
MYBPC3 gene information from NCBI.